Cancer Care
Cancer Care at Watling Street Primary Care Network
Cancer affects us all. Delivering the best outcomes for cancer patients is an absolute priority; we want every person with cancer to have the very best diagnosis, treatment and care.
YouTube Video- The NHS Long Term Plan & Commitments for Cancer

Community Support & Drop-In

🌿Living Beyond Cancer – Community Support & Drop-In Dates🌿
Join us for our next Living Beyond Cancer Support Group meeting on 4th December💚
Connect with others, share your experiences, and hear from our Guest Speaker, Michelle, Macmillan Lead Cancer Nurse at Milton Keynes Cancer Centre, as she talks about the Cancer Care Pathway.
Partners, friends, and carers are very welcome. Light refreshments are provided 💚
Kathak Elixir
A new free dance programme for adults living with and beyond cancer, in partnership with Pagrav Dance. Kathak Elixir explores Indian classical dance to support physical activity, creativity, and community. No dance experience is needed💃💚 Sessions take place on Fridays from 11am – 12pm at The Drawing Room, Westbury Arts Centre, Foxcovert Road, Shenley Wood, Milton Keynes, MK5 6AA.
OUH Macmillan Radiotherapy Late Effects Service
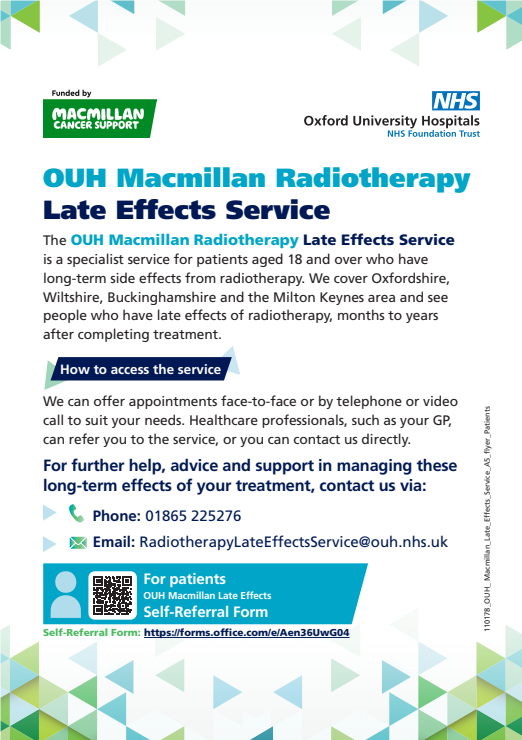
The team, who care for people across Milton Keynes, Swindon, Oxfordshire, and parts of Buckinghamshire, runs clinics at the OUH-run radiotherapy centre at Milton Keynes University Hospital.
Adults who have been treated for cancer with radiotherapy can now benefit from a new specialist service that supports them with any long-term consequences.
Although radiotherapy is an effective treatment for many types of cancer and many people make a full recovery, some individuals experience ongoing physical or psychological effects months or even years after treatment has finished.
The OUH Macmillan Radiotherapy Late Effects Service is provided by Oxford University Hospitals NHS Foundation Trust (OUH) and funded by Macmillan Cancer Support.
The service has been open to internal OUH referrals since August 2024. As of last month, patients can now self-refer or be referred by their GP.
Appointments for adults (aged 18 years and over) are offered in person, over the phone, or as a video consultation, to suit different patients' needs. People will be seen by the team as many times as required to manage their symptoms.
Self- Referral Form: https://forms.office.com/e/Aen36UwG04
Screening
Cancer screening is looking for cancer before a person has any symptoms. Screening tests can help find cancer at an early stage, before any symptoms appear. When abnormal tissue or cancer is found early, it may be easier to treat or cure.
It is important that when you're called for any cancer screening, whether it is routine, or your doctor suggests you go for screening, that you attend.
Screening tests have many goals:
- Finds cancer before symptoms appear
- Screens for a cancer that is easier to treat and cure when found early
- Has few false-negative test results and false-positive test results
- Decreases the chance of dying from cancer
Please note that screening tests do not usually diagnose cancer. If a screening result is abnormal, you may get sent for further testing to detect if the abnormality is cancer.
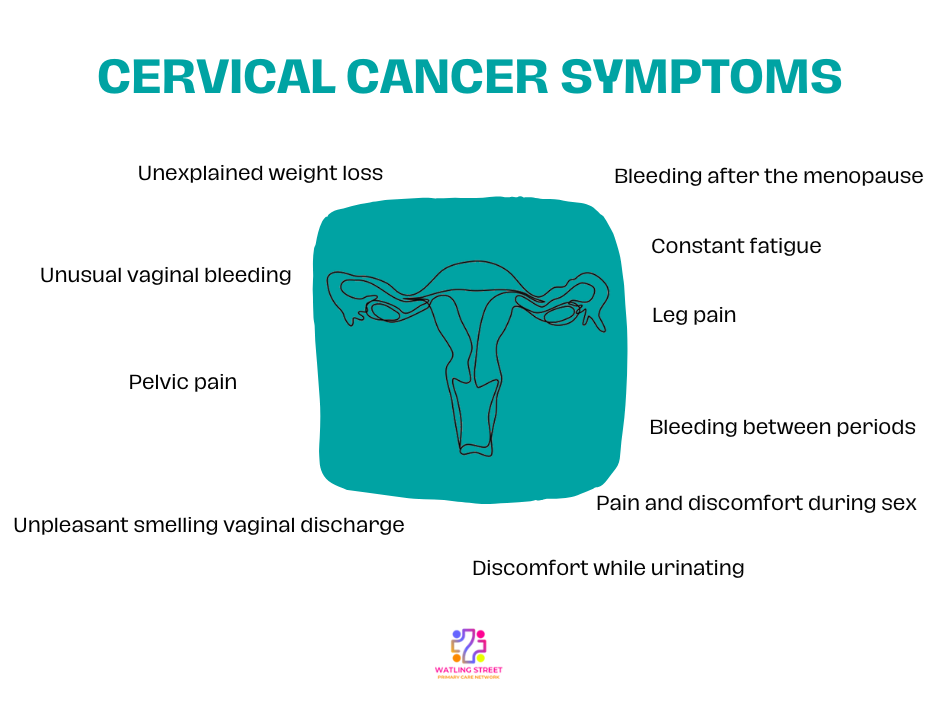
Cervical Screening
There are around 3,200 new cervical cancer cases in the UK every year, that's nearly 9 every day.
The NHS cervical screening programme in England is offered to people with a cervix aged from 25 to 64. Routine screening is offered every three years up to 49 years of age and every five years from 50 to 64 years of age. Depending on the result of the screen, people may be recalled earlier than these routine intervals.
As part of the NHS Cervical Screening Programme, all samples taken at cervical screening appointments are now being tested for high risk Human Papillomavirus (HPV) in the first instance. This is the virus which causes nearly all cervical cancers. Samples that test positive for HPV will then go on to be further analysed with Liquid Based Cytology to detect cell abnormalities. The new test will identify more people at risk of cervical cancer earlier and could prevent around 600 additional cancers a year.
HPV is a very common virus which effects around 8 in 10 people; it is nothing to be embarrassed about, and in many cases, your immune system will naturally get rid of HPV.
For more information on the cervical screening programme, please visit the NHS cervical screening pages
Breast Screening
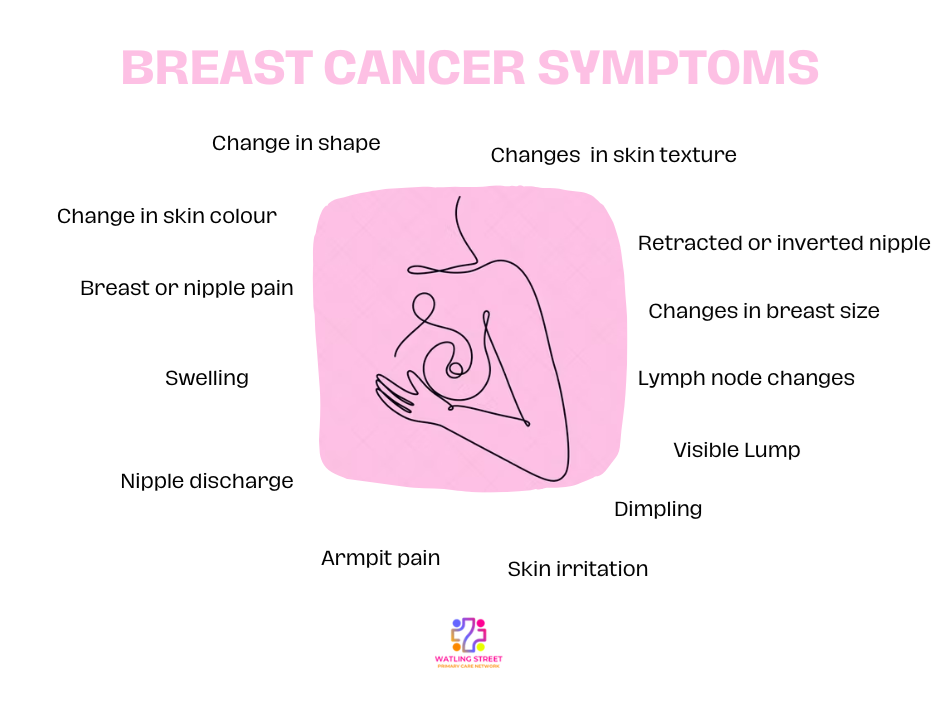
About 1 in 7 women in the UK are diagnosed with breast cancer during their lifetime. If it’s detected early, treatment is more successful and there’s a good chance of recovery.
Breast screening uses an Xray test called a mammogram that can spot cancers when they’re too small to see or feel.
Breast screening is offered to women aged 50 to their 71st birthday in England. You’ll first be invited for screening within three years of your 50th birthday.
If you are 71 or over, you will stop receiving screening invitations. You can still have screening once you are 71 or over if you want to and can arrange an appointment by contacting your local screening unit.
If you’re worried about breast cancer symptoms do not wait to be offered screening, see your GP.
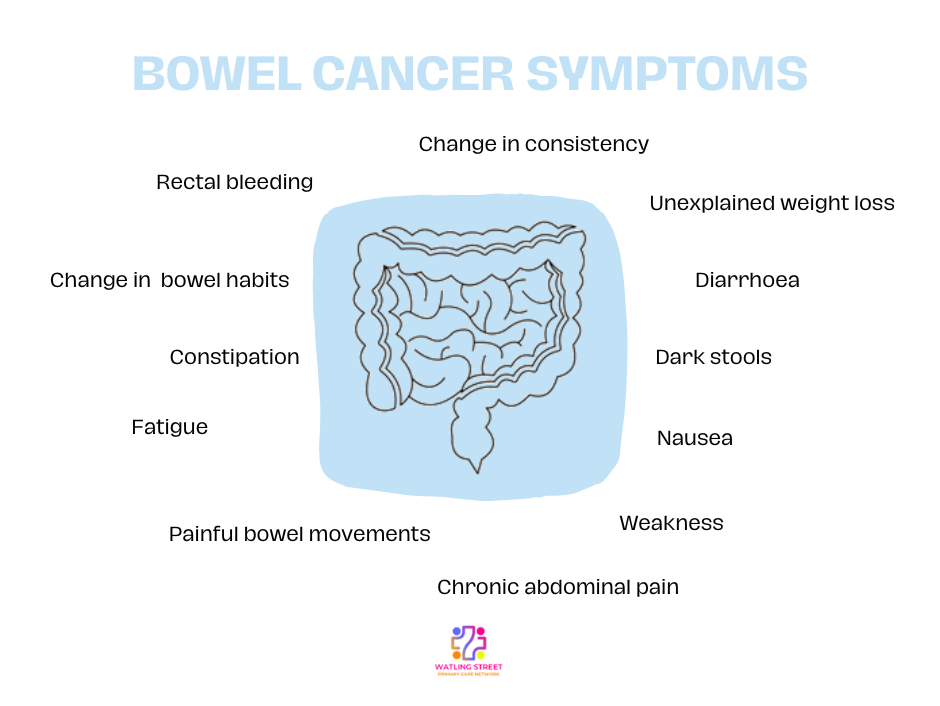
Bowel Screening
Bowel cancer is the 4th most common type of cancer. Screening can help prevent bowel cancer or find it at an early stage, when it's easier to treat.
Bowel cancer survival is improving and has more than doubled in the last 40 years in the UK. If diagnosed early, more than 90% of bowel cancer cases can be treated successfully.
Screening programmes test to see if people show any early signs of cancer. By detecting bowel cancer at an early stage, treatment has a better chance of working.
As part of the NHS Bowel Cancer Screening Programme, men and women aged 60-74 are sent a home testing kit every two years to collect a small sample of poo to be checked for tiny amounts of blood which could be caused by cancer.
Urgent Cancer Pathway
The NHS has created a useful easy-read leaflet which shows the pathway of cancer screening.
Guide to NHS Waiting Times
Your waiting time starts from whe the hospital, or service you have been reffered to recieves your referral letter, or when you book your first appointment through the NHS e-Referral Service.
During this period you may:
- Have tests, scans or other procedures to help ensure that your treatment is appropriate for your condition.
- Have medicine or therapy to manage your symptoms until you start treatment.
- Be referred to another consltant or department.
Your waiting time ends if a clinican decides no treatment is neccessary, if you decide you do not want to be treated, or when your treatment begins.
This could include:
- Being admitted to hospital for an operation or treatment.
- Starting treatment that does not require you to stay in hospital, such as taking medication.
- Beginning fitting for a medical device, e.g- leg braces.
- Agreeing to have your condition monitored for a time to see whether you need further treatment.
- Receiving advice from hospital staff about how to manage your condition.
If you're waiting for a hospital appointment or treatment, you can use the My Planned Care website to check the waiting times at your hospital.
Maximum waiting times for non-urgent referrals
The maximum waiting time for non-urgent, consultant- led treatments is 8 weeks from the day your appointment is booked through the NHS e-Referral Service, or when the hospital or service receives your referral letter.
The 18 week referral waiting time does not apply if:
- You choose to wait longer.
- Delaying the start of your treatment is in your best clinical interests, such as stopping smoking or losing weight.
- It is clinically appropriate for your condition to be actively monitored in secondary care without clinical intervention or diagnostic procedures at that stage.
- You fail to attend appointments that you had chosen from a set of reasonable options.
- The treatment is no longer necessary.
Maximum waiting times for urgent cancer referrals
The maximum waiting time for suspected cancer referral is 2 weeks from the day your appointment is booked through the NHS e-Referral Service, or when the hospital or service receives your referral letter.
For further information on NHS waiting times, please visit: Guide to NHS waiting times in England
Cancer Care at Milton Keynes Hospital
Milton Keynes Hospital Cancer Care Walkthrough Video Collection
We’re pleased to share this helpful video series created by Milton Keynes Hospital to support patients, families, and carers through their cancer care journey. The collection provides a clear and reassuring insight into what to expect when receiving treatment at the hospital. All videos are available to watch at your convenience, as often as needed.
The series includes:
-
Cancer Unit Walkthrough – A guided tour of the cancer care facilities at Milton Keynes Hospital.
-
Having a Scan – An overview of the scan process, including what happens and what the environment is like.
-
Meet the Team – Interviews with hospital staff, helping viewers get to know the professionals involved in their care.
-
Meet the Patients – Real experiences shared by patients who have undergone treatment at Milton Keynes Hospital.
Page created: 15 March 2022